When an Infection Won’t Quit: How Chronic Infections Start and Why Culture Might Miss Them
Most infections start the same way: you feel off, you see your doctor, maybe you’re prescribed antibiotics, and with any luck, the infection clears up. That’s how it’s supposed to work. But for some people, the story doesn’t end there. Instead, the infection lingers. It comes back. It never fully goes away. And despite multiple rounds of treatment, something still isn’t right.
At Bacteria Beyond Borders, we work with patients who have been fighting infections for months or even years. Often, they’ve been told over and over that their test results are normal or that no infection is present—yet their symptoms persist. In many cases, it’s not that the infection isn’t real. It’s that the standard methods for detecting it just aren’t good enough.
Let’s start with how infections begin. Bacteria or fungi enter the body through a vulnerable spot—maybe a surgical site, a urinary catheter, or just a small wound. If your immune system and the right treatment step in quickly, the invaders are cleared and the tissue heals. But sometimes, the microbes stick around. They find a way to survive—often by forming protective layers called biofilms that shield them from both your immune system and antibiotics. Think of biofilms as microscopic bunkers. The germs hunker down, slow their growth, and become much harder to kill.
Over time, these bacteria can shift into what’s called the “viable but non-culturable” (VBNC) state. They’re alive, still capable of causing trouble, but they’re dormant and can’t be grown in a lab using standard culture techniques. That’s one reason why a patient might have all the signs and symptoms of infection, yet the culture report comes back negative. It doesn’t mean there’s no infection—it just means the tools being used aren’t picking it up.
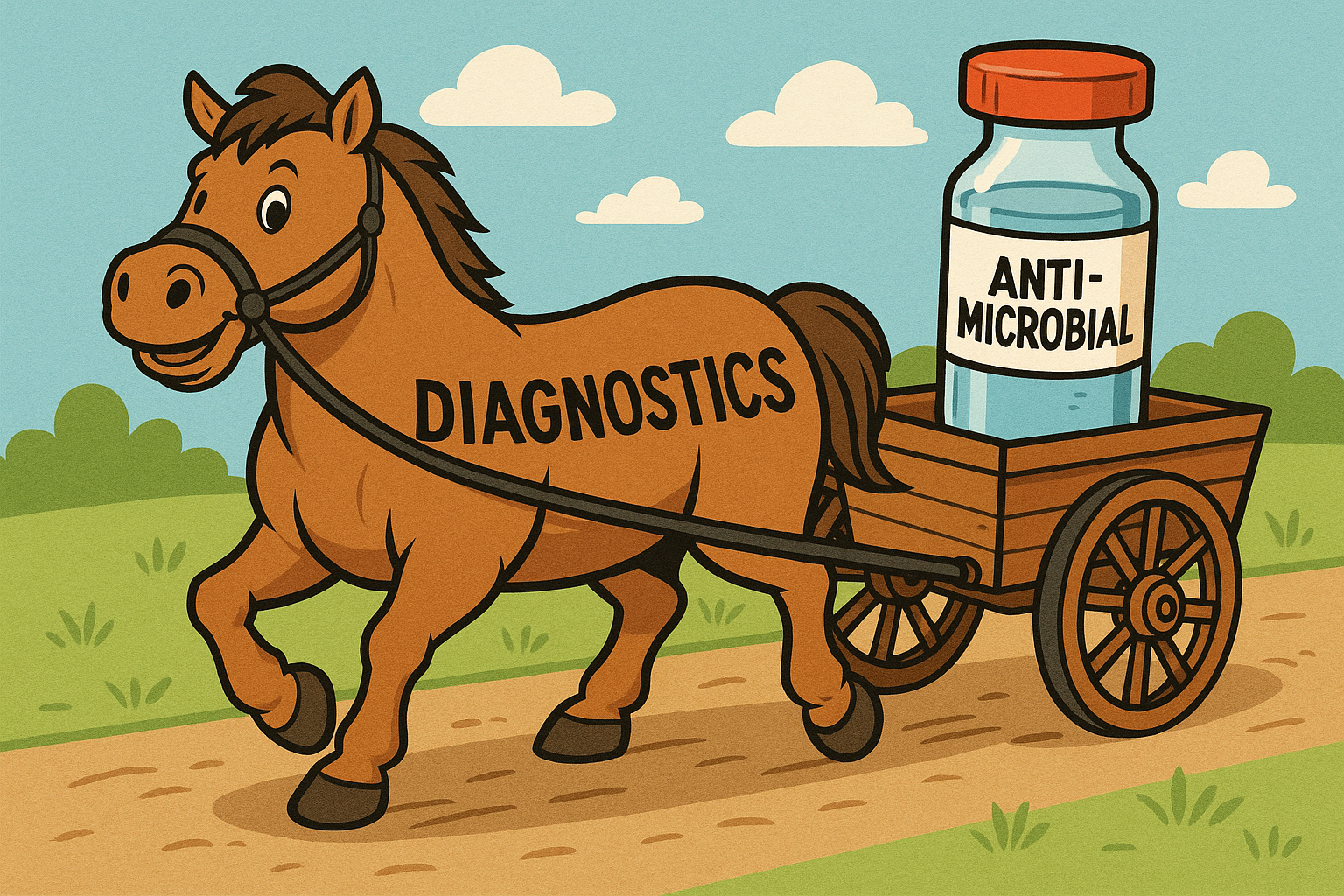
Another factor that turns an acute infection into a chronic one is when the wrong antibiotics are prescribed—either because the true pathogen was missed or because only the most easily grown bacteria were identified. In many standard lab tests, the organisms that grow best get all the attention, even if they’re not the ones actually causing the infection. Meanwhile, the real culprits—slow-growing, anaerobic, or biofilm-protected microbes—remain undetected and untreated. Over time, the infection becomes harder to treat, and the immune system may become exhausted or desensitized to the chronic threat.
This is where next-generation sequencing, or NGS, comes in. Instead of trying to grow microbes, NGS analyzes the DNA in the sample to see what organisms are present. It doesn’t rely on how well something grows in a dish. If it’s there—alive or recently active—
NGS can detect its genetic fingerprint. That gives doctors a much more complete picture of what’s going on, especially when traditional tests fail.
At Bacteria Beyond Borders, we help patients access this advanced diagnostic testing. We begin by reviewing a patient’s history—how the infection started, what treatments were tried, and what symptoms remain. We then facilitate NGS testing through MicroGenDX, a leading clinical laboratory. If the results point to a persistent or difficult-to-treat infection, we connect the patient with a licensed physician who can interpret the findings and guide treatment. We also connect patients and physicians to reputable specialty compounding pharmacies in case they are able to treat the infection topically.
In cases involving drug-resistant bacteria, phage therapy may be considered. Phages are viruses that infect only bacteria—not human cells—and they can be selected to target the exact strains of bacteria found in the infection. While not yet widely available, phage therapy has shown promise in treating chronic, antibiotic-resistant infections that nothing else can touch.
If your cultures have been negative but your symptoms haven’t gone away, you are not alone—and you are not imagining things. A negative culture doesn’t rule out infection. It only rules out bacteria that can grow under specific lab conditions. Understanding this simple fact can change everything about how chronic infections are diagnosed and treated.
If you’ve been stuck in this cycle, or you know someone who has, Bacteria Beyond Borders is here to help. We believe every patient deserves a clear answer—and a shot at getting their life back.
Please reach out to us for help!