What is Methicillin Resistance and Why Should You Care?
You may have heard of the term “MRSA” before—it stands for Methicillin-Resistant Staphylococcus aureus, and it’s a type of bacterial infection that is resistant to many common antibiotics, including methicillin. But what does methicillin resistance really mean, how does it happen, and why is it such a concern?
Let’s break it down in easy-to-understand terms.
What is Methicillin Resistance?
Methicillin is a type of antibiotic that was once very effective at treating infections caused by Staphylococcus aureus, a common bacterium. However, over time, some strains of Staphylococcus aureus developed the ability to survive even when methicillin was used to treat them. These strains are what we now call “methicillin-resistant.”
Methicillin resistance doesn’t just mean bacteria are resistant to methicillin. It also means the bacteria are resistant to an entire class of antibiotics called beta-lactams. This includes:
· Penicillin
· Amoxicillin
· Oxacillin
· Cephalosporins (such as cefazolin or cephalexin)
So, when a bacterial strain is classified as methicillin-resistant, it’s essentially resistant to many of the most commonly used antibiotics for treating infections. This makes MRSA much harder to treat.
A Bit of History: From Methicillin to Oxacillin
Methicillin was introduced in the 1950s as a solution to penicillin-resistant Staphylococcus aureus. Unfortunately, it wasn’t long before methicillin resistance also developed. While methicillin was effective for a time, it had some drawbacks, particularly in how it was broken down by the body. For this reason, it’s no longer widely used in clinical practice.
In place of methicillin, oxacillin and other related antibiotics (like nafcillin) were developed and are used more commonly today. Despite this, the term “methicillin-resistant” is still used to describe these strains of bacteria. So, when we talk about MRSA, we’re referring to bacteria that are resistant to a broad range of beta-lactam antibiotics, including oxacillin.
How Does Methicillin Resistance Develop?
Bacteria, like all living organisms, are always evolving. When antibiotics like methicillin are used to kill bacteria, there’s a chance that a few of them might survive due to random genetic changes (mutations). These resistant bacteria can then multiply and spread, making future infections harder to treat with the same antibiotics.
Over time, the more antibiotics are used, the more chances bacteria have to develop resistance. That’s why methicillin, which was once effective, is no longer able to stop certain strains of Staphylococcus aureus. These strains have essentially “learned” how to survive methicillin treatment.
How is Methicillin Resistance Treated Today?
Even though MRSA is resistant to methicillin and other common antibiotics, there are still treatments available. Doctors typically turn to stronger, more targeted antibiotics, such as:
· Vancomycin
· Linezolid
· Daptomycin
· Clindamycin
However, these antibiotics can have more side effects, and in some cases, the bacteria may also develop resistance to them. Treating methicillin-resistant infections requires careful monitoring, and patients often need to be isolated to prevent the infection from spreading to others.
How Many People Are Affected by Methicillin Resistance?
MRSA is a major global health issue. According to the Centers for Disease Control and Prevention (CDC), more than 2.8 million antibiotic-resistant infections occur in the United States each year, leading to at least 35,000 deaths. Of these, about 20,000 deaths are attributed to MRSA infections alone.
While MRSA infections are particularly dangerous in hospitals and nursing homes, they can also occur in the general community. This is why practicing good hygiene, like washing hands and cleaning wounds, is so important in preventing the spread of resistant bacteria.
What Can You Do to Help Prevent the Spread of Resistance?
· Use antibiotics only when prescribed by a healthcare provider. Taking antibiotics unnecessarily, such as for viral infections, increases the chances of bacteria developing resistance.
· Complete your full course of antibiotics. Even if you feel better, stopping treatment early can leave some bacteria alive, giving them a chance to become resistant.
· Practice good hygiene. Wash your hands regularly and keep cuts and wounds clean to reduce the risk of infections.
· Don’t share antibiotics. Antibiotics are prescribed based on specific infections, and using someone else’s prescription can contribute to the development of resistance.
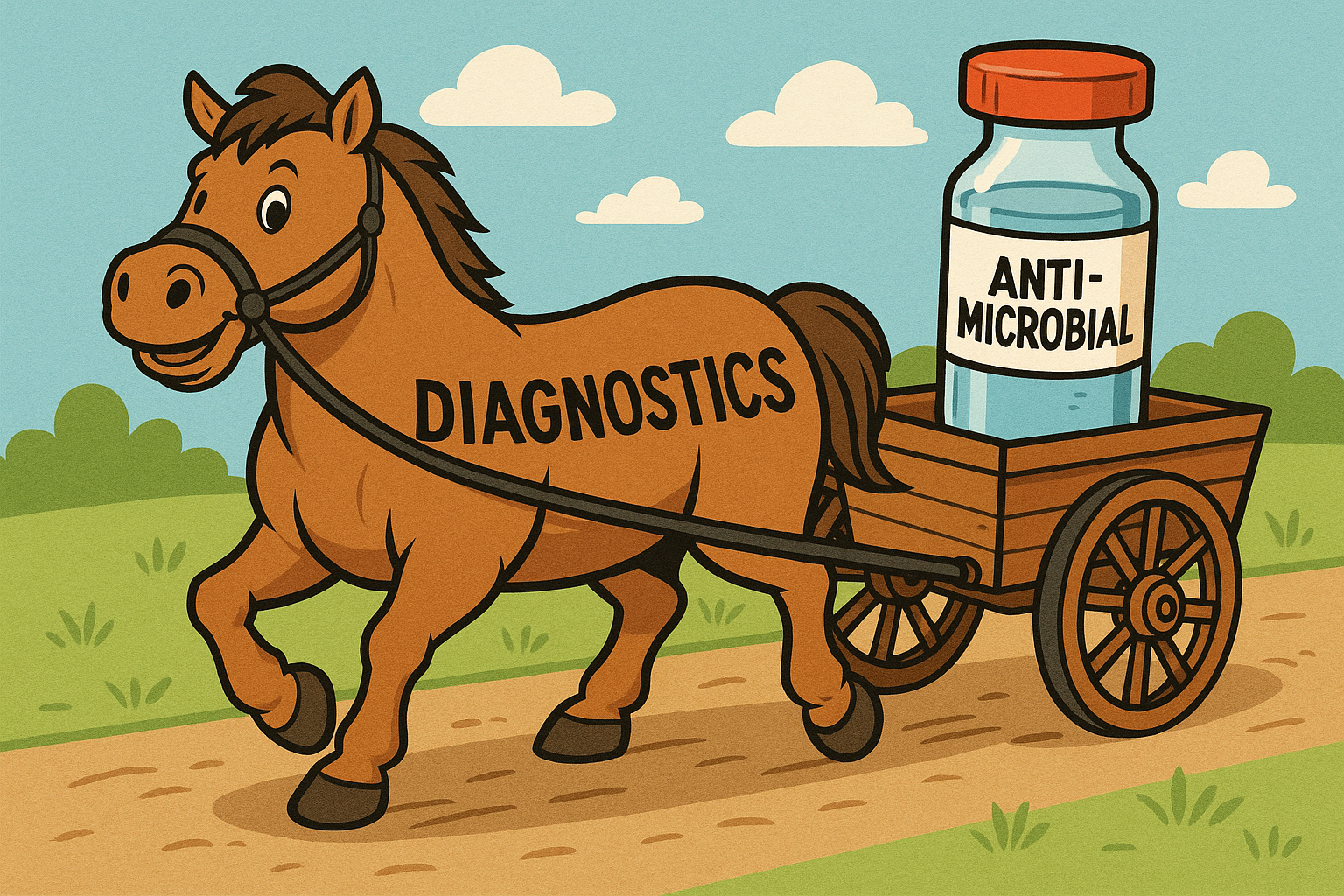
· Educate yourself about advanced diagnostic testing. Some diagnostic tools, such as those offered by MicroGen DX, can identify exactly which bacteria are causing an infection and whether they are resistant to certain antibiotics. By learning about these tests, you can advocate for them when talking to your physician. This helps ensure treatments are tailored to your specific infection, reducing the chances of ineffective treatment and further resistance.
The Bottom Line
Methicillin resistance is a serious and growing problem, but understanding how it works can help us fight back. By using antibiotics wisely and following good hygiene practices, we can help slow the spread of resistant bacteria and protect the effectiveness of the medications we rely on.
If you’d like to learn more about antibiotic resistance and how you can help, visit www.bacteriabeyondborders.org