Life changed by infection: a story of one fight
Many of us regularly hear about antimicrobial resistance (AMR) from the news, from health campaigns, or even at the pharmacy. Despite this, it often remains a somewhat distant problem that we don’t face in daily life. It is something that is happening elsewhere to someone else.
Today, we are sharing the story of one family directly and unexpectedly impacted by antimicrobial resistance, whose lives have been divided into “before” and “after” ever since.
It all started as a minor and uneventful illness which many of us have had numerous times in our lives and recovered from. On Mother’s Day in 2011, Addie Rerecich, then a healthy 11-year-old girl from Tucson, Arizona, started to feel a bit more tired than usual. Her mom, who was a nurse, did not think of it as anything serious since Addie had been an active kid who enjoyed playing sports and attributed the fatigue to exhaustion. About a week later, Addie started complaining of hip pain, which her mom thought was likely caused by a pulled muscle, and booked a doctor’s appointment for the next day. However, Addie never made it to that appointment and had to be rushed to a local ER instead that same night with a 103°F fever.
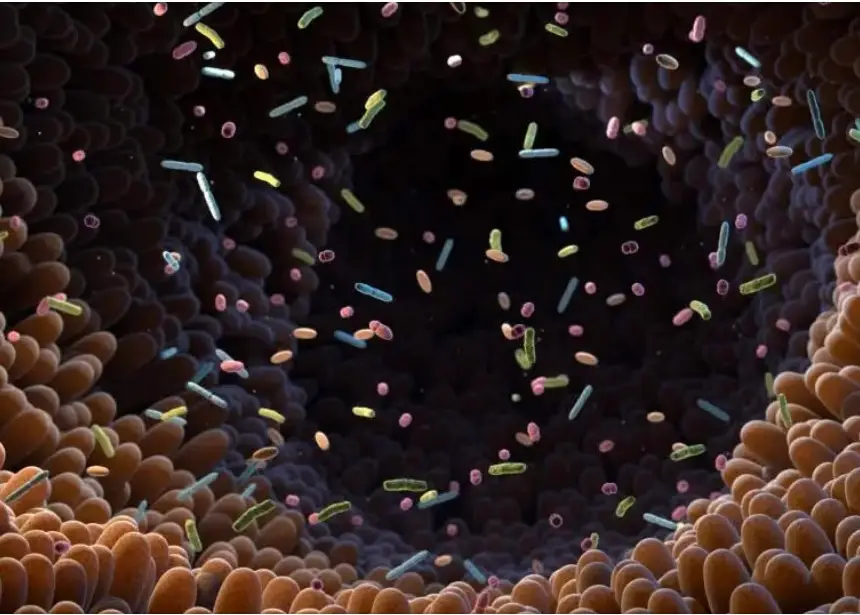
The fever turned out to be caused by an abscess deep inside Addie’s hip muscle. The infection then spread from the abscess throughout her body, including the lungs, causing severe pneumonia. The culprit was methicillin-resistant Staphylococcus aureus, or MRSA – a resistant microbe known to cause infections inside hospitals, which has become a common cause of illness in the community as well, sometimes affecting healthy people who were never hospitalized. In Addie’s case, the infection likely entered her body through a small scab but then spun out of control and she, an otherwise healthy child, had to spend five months in the hospital fighting for her life.
The pneumonia damaged the lungs so severely that Addie had to be put on ECMO – a machine that completely replaces lung function to deliver oxygen to the body. Unfortunately, this life-saving treatment came with more complications – while in the hospital, Addie got infected by other bacteria. This time the bacteria were a different kind – multidrug-resistant hospital-acquired ones. In hospitals, where bacteria are frequently exposed to antibiotics, they often develop resistance to multiple drugs and cause severe infections in vulnerable patients, such as the ones in the ICU, often entering through tubes and lines connected to the body. Since these microbes were resistant to almost all drugs, doctors had to resort to treating Addie with an antibiotic called Colistin – an effective but very toxic one that has side effects on the kidneys, nervous system, and other organs. Because of its toxicity, Colistin is often considered to be a “last-resort” drug used when safer antibiotics don’t work.
When Addie was finally discharged from the hospital, she was in a wheelchair. Once a healthy and active child, she had to learn to walk again. Her lungs were damaged so badly that she required a lung transplant. The medical costs of Addie’s hospital stay topped $6 million, and after discharge, despite having health insurance, her family continued to pay significant fees for medications and doctor visits. Sadly, less than a decade later, Addie’s body started rejecting the lung transplant she had received in 2011. She made a difficult decision not to undergo another transplant and passed away in December 2019, aged 20.
Addie’s mother Tonya was in the hospital day and night during the five months of her admission, and both she and Addie’s dad had to be on an unpaid leave from work, relying on donations for support. She later had to overcome alcohol and drug use from PTSD caused by her daughter’s illness.
The story of Addie Rerecich and her family is not just one of illness – it is also a story of incredible strength and resilience in the face of antimicrobial resistance, and healing after losing a loved one. It reminds us that antimicrobial resistance isn’t someone else’s problem — it’s everyone’s responsibility. Resistant microbes are present not only in hospitals but in the community where we live. The good news is that we are not powerless: we can take steps together to protect the effectiveness of antibiotics and limit the global threat of AMR.