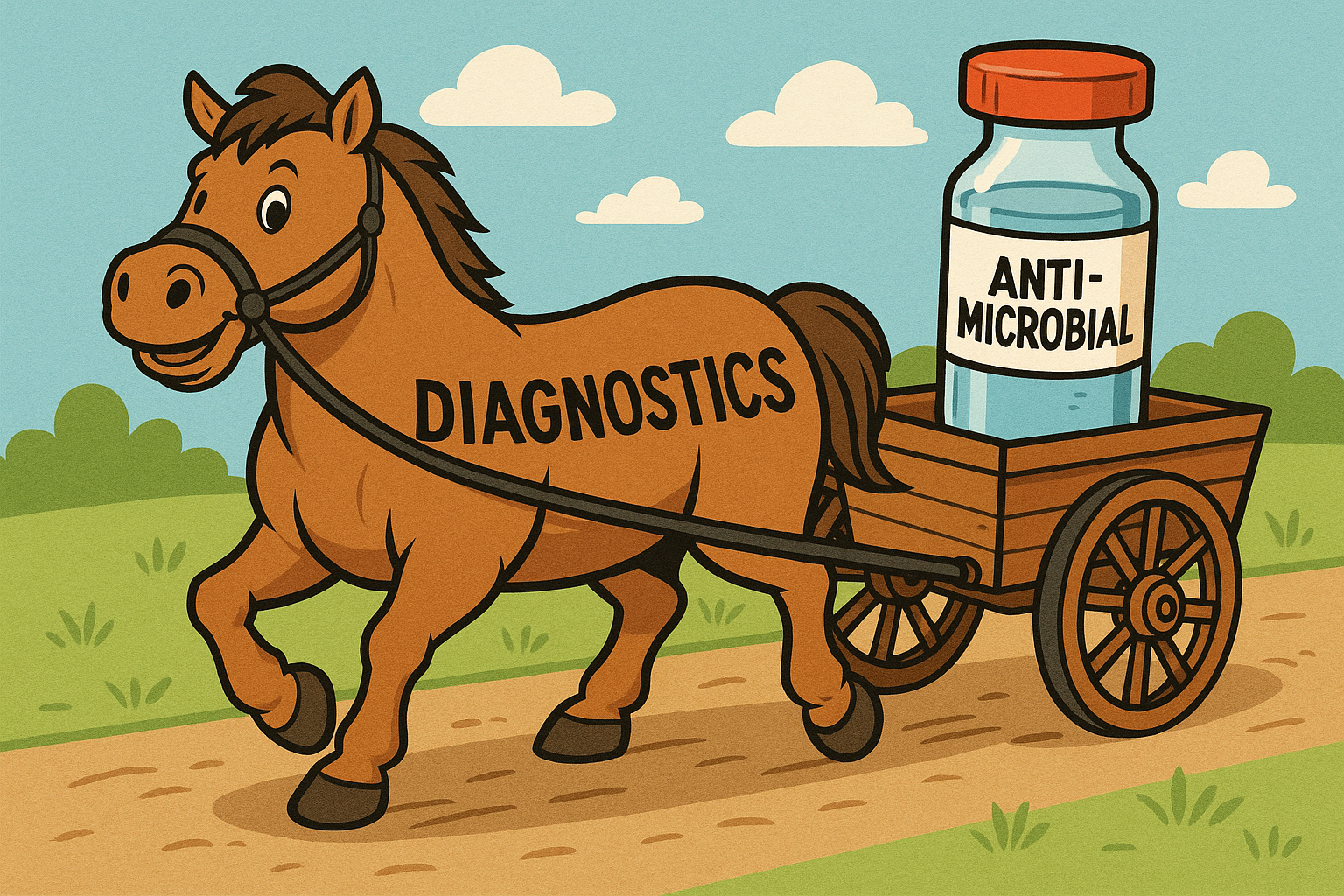
Diagnostic Stewardship: Letting the Horse Pull the Cart
The road ahead: The Rise of AMR and Superbugs
Antimicrobial resistance (AMR) is not a modern invention. It is evolution in fast forward. Every time bacteria encounter antibiotics, the susceptible die and the resistant survive. Over time, that survival pressure transforms the microbial landscape.
Imagine a weekly endurance challenge where only the fittest competitors remain in the game. Those who falter are replaced, but those who endure grow stronger each week. The principle drives resistance: antibiotic exposure becomes a training ground, and the winners – the resistant bacteria – multiply.
Today’s “superbugs” like Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococcus (VRE), Carbapenem-resistant Acinetobacter baumannii (CRAB), and Clostridioides difficile have turned that evolutionary marathon into a global crisis. Many pathogens now resist multiple drugs, forcing physicians to use older, more toxic antibiotics. Meanwhile, pharmaceutical innovation has stalled under economic and regulatory strain. The result is a widening gap between what infections demand and what medicine can deliver.
But AMR is not confined to hospital walls. Agriculture accounts for a large share of global antibiotic use, where low-dose exposures for growth promotion and disease prevention drive resistance on a massive scale (You and Silbergeld, 2014). Resistant bacteria spread through food, soil, and water, quietly migrating from farm to table. This reality demands a One Health approach which recognizes the connectedness between human, animal, and environmental health.
Inside the clinic, the problem compounds. Public health campaigns tell patients to “finish your antibiotics,” but adherence is only part of the story. The deeper issue is empiric prescribing or starting antibiotics without a data-driven diagnosis. It could also be called educated guessing. Guma et al. (2022) found that more than half of general practitioners prescribe empirically, or guess, over 70% of the time, primarily for symptom relief. Why? Because culture-based diagnostics are too slow or too insensitive to provide answers when decisions must be made.
Cultures miss biofilm-embedded, fastidious, or antibiotic suppressed organisms. Only about 2% of environmental bacteria and roughly half of oral microbes can be grown in routine cultures (Wade, 2002). The result is predictable: when faced with uncertainty, physicians prescribe broad-spectrum antibiotics “just in case.”
This cycle plays out daily. A patient arrives with symptoms of infection. Cultures are ordered, as guidelines dictate. When results return negative (despite clear clinical signs) the physician faces a dilemma: treat blindly or risk doing nothing. The patient wants relief; the doctor wants resolution. The prescription pad becomes the fallback. The missing ingredient isn’t intent, it’s information.
Why are we stuck here? A mismatch between vision and infrastructure
Hospitals have spent the last decade building robust antimicrobial stewardship programs (ASPs) to ensure antibiotics are used wisely. But even the best stewardship initiatives operate with an unspoken handicap: they rely on underpowered and insensitive diagnostics.
Stewardship is about precision. The right drug, at the right dose, at the right time. But precision demands clear targets. That’s where diagnostic stewardship comes in. It ensures the right test is ordered, performed, and interpreted at the right time. Without that foundation, antimicrobial stewardship becomes reactive, forced into empiricism rather than guided by evidence. When diagnostics lag, stewardship stumbles. The result? Even well-designed programs can inadvertently reinforce the very resistance they aim to prevent.
The Gold Standard That No Longer Glitters
Culture has long been medicine’s benchmark for infection diagnosis. Yet today, it’s often a bottleneck. Cultures take days to grow, miss key pathogens, and fail in the presence of antibiotics or biofilms. Despite these limitations, guidelines continue to enshrine culture as the “gold standard,” defining success by its results rather than its relevance.
The persistence of culture is not just habit, it’s infrastructure. It’s perceived to be cheap (though not always), it’s familiar, and it’s built into the regulatory DNA of hospitals and accreditation systems. But diagnostically, it’s anemic. When results arrive too late, or come back negative, clinicians are left guessing. Broad-spectrum therapy becomes the default, and the resistance cycle tightens another turn.
Studies show that diagnostic accuracy is the single strongest driver of antibiotic prescribing behavior. Yet diagnostic stewardship remains under-recognized and underfunded. In essence, the healthcare system is trying to steer the cart of antimicrobial stewardship without harnessing the horse of diagnostics.
Why Diagnostic Stewardship Must Come First
Diagnostic stewardship isn’t an optional companion to antimicrobial stewardship; it is the foundation that makes it work. The two are complementary but sequential: diagnostics first, treatment second. When diagnostics are optimized for speed, sensitivity, and clarity, stewardship programs can finally operate on data, not assumptions.
Effective diagnostic stewardship:
- Ensures the right tests are ordered for the right patients at the right time
- Reduces unnecessary or repeated cultures that muddy the clinical picture
- Provides comprehensive microbial identification through advanced, precision diagnostics for early, targeted therapy.
- Embeds best practices within laboratory and EHR workflows to ensure consistent interpretation.
In short, diagnostic stewardship gives antimicrobial stewardship something it has always needed – vision.
The Tools at Hand: Precision Diagnostics in the Fight Against AMR
Every antibiotic prescribed without diagnostic evidence risks furthering AMR. That’s why integrating advanced molecular techniques, like PCR and Next-Generation Sequencing (NGS), is essential. PCR and NGS are redefining how we diagnose infection. By identifying pathogens and their resistance genes with speed and precision, these tools enable truly targeted therapy. PCR-based panels, for example, can rapidly identify respiratory viruses, helping clinicians avoid unnecessary antibiotics. But PCR’s focus is narrow only targeting what it has been told to look for.
NGS, by contrast, takes a panoramic view. It can detect everything in the sample, cultivable or not. This makes it indispensable for complex or culture-negative infections. Commercial NGS services like MicroGenDX’s combined qPCR+NGS service exemplifies this power. Capable of identifying over 60,000 bacterial and fungal species, it can detect pathogens missed by culture and uncover dysbiosis where a single culprit alone may not be to blame. It’s especially valuable in cases like periprosthetic joint infections (Kullar et al., 2023) or chronic UTIs (Coba et al., 2019), where biofilms and fastidious organisms routinely evade culture.
In addition, MicroGenDX reports resistance genes spanning 10 antimicrobial classes, information that turns empiric prescribing into targeted treatment. For clinicians managing complex polymicrobial infections, this level of insight can mean the difference between escalation and recovery.
The Cart: Antimicrobial Stewardship
Once diagnostics lead, antimicrobial stewardship can follow. PCR and NGS give antimicrobial stewardship programs the data they need to act with confidence, escalating, de-escalating, or discontinuing therapy in real time. Consider fungal cultures, which take 28 days to return negative. NGS delivers results in 24-48 hours, allowing physicians to make informed decisions weeks sooner, minimizing exposure and maximizing precision.
Institutions like Stanford Health Care illustrate what success looks like. As an IDSA Antimicrobial Stewardship Center of Excellence and Gold Honor Roll recipient from the California Department of Public Health, Stanford integrates clinical leadership, pharmacy oversight, and advanced diagnostics to reduce unnecessary antibiotic use while improving outcomes.
New Roads: Phage Therapy – Precision Treatment for Resistant Infections
Diagnostics may guide the way, but precision therapeutics will take us the rest of the journey. Phage therapy (using viruses that infect bacteria) offers a lifeline where antibiotics fail. These naturally occurring bacteriophages destroy bacterial pathogens without disturbing the body’s healthy microbiome. The 2017 case in San Diego where phage therapy saved a patient from a multidrug-resistant Acinetobacter baumannii infection demonstrated proof of the concept.
Here again, diagnostics are the key. PCR and NGS can identify the bacterial species and resistance mechanisms needed to determine the appropriate phage. NGS can even detect fungal co-infections that might otherwise sabotage therapy. Phage therapy still faces hurdles: isolation and culturing take time, and mixed infections may require combination strategies.
Getting Down the Road: Empowering Precision Medicine
The road ahead requires more than new antibiotics. It requires a shift in mindset, from treating first to understanding first. NGS represents that shift. By revealing the complete microbial picture, including resistance genes and unculturable pathogens, it transforms infection care from reactive to data driven. Combined with stewardship programs and emerging treatments like phage therapy, it’s ushering in a new era of precision medicine.
Yet the real revolution won’t come from laboratories alone. It will come from awareness. When patients and providers alike demand diagnostic precision before treatment, the balance shifts. Each conversation that begins with “Let’s find out what’s causing this” moves healthcare closer to sustainability.
Let diagnostics lead. Let the horse pull the cart. With diagnostic stewardship at the front, healthcare can finally steer toward a future where treatment is personal, outcomes improve, and antimicrobial resistance begins to slow, one informed decision at a time.
Author: Nicholas Sanford, PhD, BCMAS
References:
- You Y, Silbergeld EK. Learning from agriculture: understanding low-dose antimicrobials as drivers of resistome expansion. Front Microbiol. 2014;5:284. doi:10.3389/fmicb.2014.00284
- Guma SP, Godman B, Campbell SM, Mahomed O. Determinants of the Empiric Use of Antibiotics by General Practitioners in South Africa: Observational, Analytic, Cross-Sectional Study. Antibiotics. 2022; 11(10):1423. https://doi.org/10.3390/antibiotics11101423
- Wade W. Unculturable bacteria–the uncharacterized organisms that cause oral infections. J R Soc Med. 2002 Feb;95(2):81-3. doi: 10.1177/014107680209500207. PMID: 11823550; PMCID: PMC1279316.
- Kullar R, Chisari E, Snyder J, Cooper C, Parvizi J, Sniffen J. Next-Generation Sequencing Supports Targeted Antibiotic Treatment for Culture Negative Orthopedic Infections. Clin Infect Dis. 2023 Jan 13;76(2):359-364. doi: 10.1093/cid/ciac733. PMID: 36074890; PMCID: PMC9839185.
- Coba G, Koo T, Zaman S, et al. MP47-07 COMPARATIVE VALUE OF CHRONIC URINARY TRACT INFECTION (UTI) DIAGNOSIS BETWEEN STANDARD CULTURE SENSITIVITY AND NEXT GENERATION SEQUENCE (NGS) IN URINE SAMPLES. J Urol. 2019;201(Supplement 4):e689-e690. doi:10.1097/01.JU.0000556319.92548.c7