Antimicrobial Resistance: A Longstanding Battle, Not a Sudden Crisis
If you’ve been following the news about antimicrobial resistance (AMR), you’ve probably heard it called the “silent pandemic.” This phrase gained traction after a Lancet study in 2022 estimated that AMR was directly responsible for 1.27 million deaths worldwide in 2019. Since then, AMR has been getting more media attention, and many people are under the impression that resistance is rapidly worsening.
Let’s be clear: AMR hasn’t suddenly gotten worse. It has been on the rise for decades—because that’s how evolution works. Granted, bacteria evolve much faster than humans, given their rapid generation times and ability to exchange genetic material like trading cards. But evolution still takes time. Resistance doesn’t just appear overnight. What has changed is our ability to detect and track AMR more effectively than ever before.
The Real Story Behind Rising AMR Reports
The reason we’re seeing more AMR-related deaths isn’t because bacteria just recently figured something out. Instead, advancements in diagnostic capabilities have allowed us to recognize and track AMR more accurately. In the past, a patient with a resistant infection might have died from what was labeled as “surgical complications” or “multiorgan failure” without anyone realizing that a drug-resistant pathogen was the true cause.
You might say, “The COVID-19 pandemic led to an increase in antibiotic misuse, especially in hospitalized patients” or that, “The globalization of healthcare has facilitated the spread of resistant bacteria across borders faster than before, or maybe, “the overuse of last-resort antibiotics like carbapenems and colistin has intensified selection pressure, leading to more extreme resistance patterns in a short period.”
While these factors may have temporarily increased the rate of resistance in some settings, they are not the root cause of AMR. The fundamental driver of bacterial AMR is bacterial evolution which is ongoing and cumulative. Short-term events may highlight or amplify the problem, but they don’t create AMR in a vacuum.
Another counterargument might be that AMR has accelerated because we haven’t developed enough new antibiotics to keep up with resistance. Since the golden age of antibiotic discovery (~1940’s-1970’s), pharma companies have dramatically slowed down development of new antimicrobials and instead of cycling through novel antimicrobials, we’ve been relying on the same classes of drugs for decades, increasing the likelihood that resistance will develop and spread.
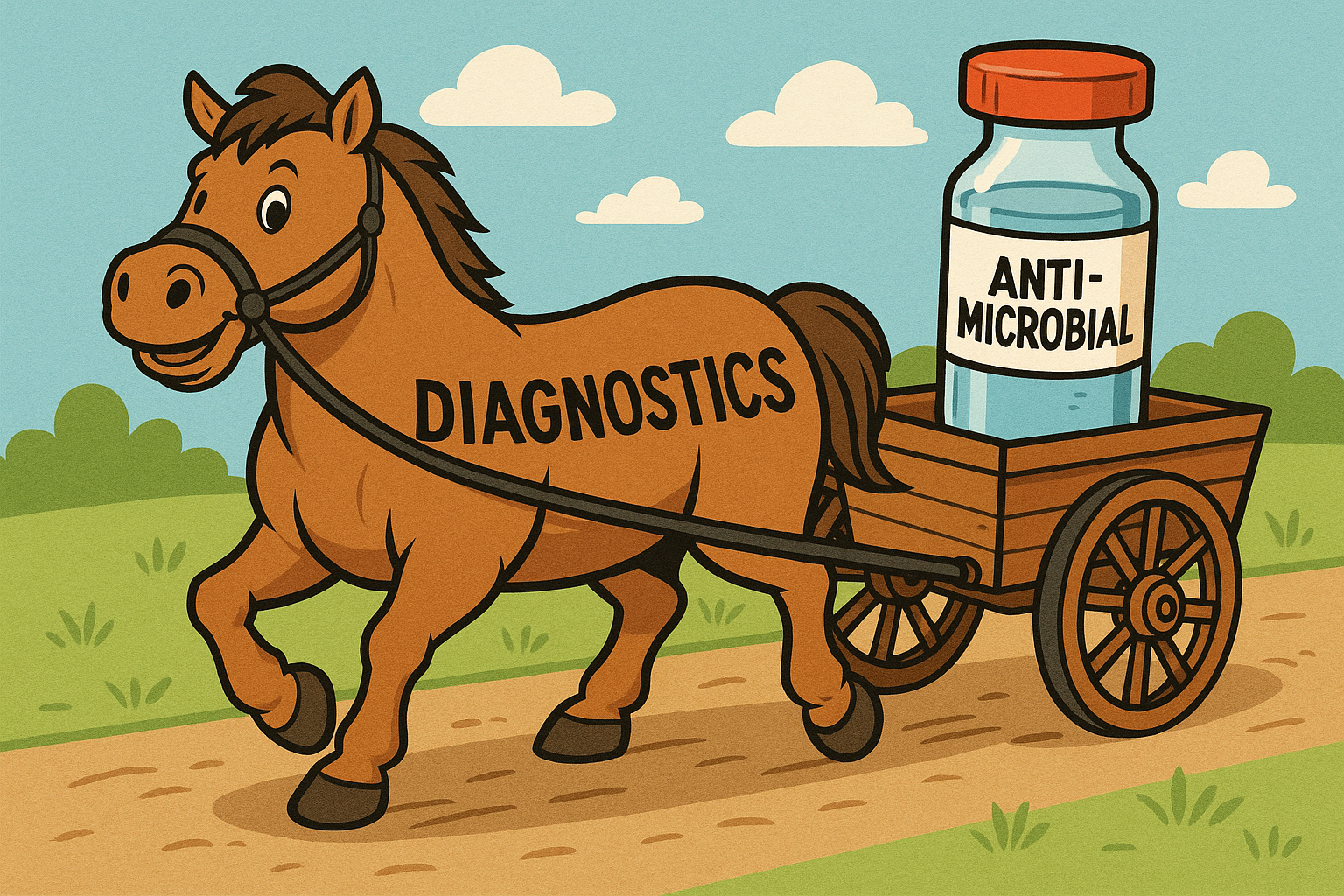
While all of this is partially true, it doesn’t change the fact that AMR is an evolutionary process, not a sudden crisis, as AMR would have still developed even with new antibiotics because of how we use them. Even with a continuous pipeline of new antimicrobials, resistance would still emerge because bacteria adapt to selection pressure over time. Overuse and misuse of antibiotics in human medicine, agriculture, and livestock production have driven AMR faster than drug discovery could realistically counteract. Even if we had ten brand-new antibiotic classes today, resistance would still develop unless we also improve diagnostics, infection prevention, and stewardship strategies. A better solution wouldn’t be just throwing more antibiotics into the mix, it would be advancing precision medicine, where rapid diagnostics guide antibiotic use, reducing unnecessary prescriptions and slowing resistance development.
Today, molecular diagnostics, next-generation sequencing (NGS), and improved clinical awareness are helping us connect the dots. What looks like a dramatic increase in AMR-related deaths is, in many cases, simply better data collection. We’re no longer misclassifying these deaths—we’re identifying them for what they really are.
How AMR Is Detected Today
Traditionally, AMR is diagnosed using antimicrobial susceptibility testing (AST), where bacteria are cultured from a patient sample and exposed to various antibiotics to determine which ones still work. This method has been the gold standard for decades, and while it sounds simple in theory, in practice, it’s anything but.
To run an AST, you first must isolate the organism in culture. That alone is a challenge. We can only grow about 2% of the bacteria we know exist using routine cultures. Even when an organism is known to grow in culture, it often refuses to cooperate. Lab conditions must be just right—appropriate media, precise atmospheric conditions, and a bit of luck that the bacteria aren’t in a viable-but-not-culturable (VBNC) state.
These limitations lead to false negatives — in some cases, up to 30-80% of the time depending on the sample type. If the bacteria don’t grow, AST results are impossible to obtain. Additionally, organisms growing in biofilms are often unrecoverable in culture. Considering the NIH statement that 60-85% of infections are biofilm associated, determining the presence of AMR with the current gold standard could leave a lot of gaps in the data.
Molecular diagnostics are starting to fill these gaps. PCR and other molecular methods can detect resistance genes directly from a sample, sometimes within hours. Unlike AST, they don’t require waiting for bacteria to, maybe, grow. Instead, they look for genetic markers that encode resistance, such as:
- mecA → MRSA (methicillin-resistant Staphylococcus aureus)
- NDM-1 → Carbapenem resistance
- vanA → Vancomycin-resistant Enterococcus (VRE)
While molecular methods don’t yet replace AST in every scenario, they provide faster answers, allowing for more immediate and targeted treatment decisions, especially for suspected multidrug-resistant infections.
But can’t PCR miss novel resistance mechanisms such as resistance due to mutations in previously unknown genes and functional resistance mechanisms that don’t always correlate with known genetic markers?
A valid point, but it doesn’t diminish the value of molecular diagnostics. PCR and sequencing provide a major advantage in speed and sensitivity, especially in culture-negative patients and patients with biofilm-associated infections. For unknown or emerging resistance mechanisms, NGS and metagenomics can help by identifying novel mutations and gene cassettes that traditional PCR panels will likely miss. Additionally, as sequencing databases grow, we will continue to refine our ability to detect genetic signatures encoding resistance.
That said, a combined approach (using molecular testing alongside traditional AST where needed) is likely the best path forward – at least for now.
The Future: Predicting Resistance with 100% Accuracy
Right now, we’re at a turning point where sequencing technology is becoming faster, cheaper, and more accessible. Soon, we may no longer need cultures at all to determine antimicrobial susceptibility. Instead, whole-genome sequencing (WGS) could provide a complete resistance profile just from bacterial DNA.
Imagine a world where, instead of waiting days for culture-based AST results, a patient’s infection is sequenced immediately, and within hours, we know:
✅ Exactly which antibiotics will work
❌ Which ones will fail
🔬 How the bacteria might evolve resistance further
This is the future of AMR diagnostics. We’re not quite there yet, but researchers are rapidly advancing machine learning and AI-driven models that predict antimicrobial susceptibility directly from genomic data. Once these tools become mainstream, we may eliminate the trial-and-error approach to prescribing antibiotics, improving both patient outcomes and antibiotic stewardship.
What This Means for Patients
For patients battling AMR infections, the best thing you can do is advocate for the most advanced diagnostics available. If you or a loved one is facing a persistent infection, ask about molecular testing options like PCR and next-generation sequencing. Reach out to Bacteria Beyond Borders so we can assist you.
AMR isn’t a new problem, but our ability to detect and fight it is evolving. The more we understand it, the better we can advocate for solutions that will save lives.
Final Thoughts & Call to Action
If you or someone you know is dealing with a serious infection that isn’t responding to antibiotics, speak up! Many hospitals and physicians are still relying on outdated diagnostic methods. The more we push for better diagnostic tools; the sooner AMR becomes a solvable—not silent—pandemic.
Author: Nicholas Sanford, PhD, BCMAS